Types Of IUDs
IUDs, or intrauterine devices, are a type of birth control that are inserted into the uterus to prevent pregnancy. There are two main types of IUDs: hormonal and non-hormonal. Hormonal IUDs release progestin, a hormone similar to progesterone, to prevent pregnancy, while non-hormonal IUDs are made of copper and prevent pregnancy by creating an inflammatory response that is toxic to sperm.
IUDs are one of the most effective forms of birth control available, with a failure rate of less than 1%. They are also a long-acting form of birth control, with some types lasting up to 10 years. Unlike other forms of birth control, IUDs do not require daily attention, making them a convenient option for many women.
When considering an IUD, it is important to understand the different types available, as well as the benefits and potential side effects of each. Additionally, it is important to discuss any medical conditions or concerns with a healthcare provider to determine if an IUD is the right choice for you.
Key Takeaways
- IUDs are a highly effective and long-acting form of birth control.
- There are two main types of IUDs: hormonal and non-hormonal.
- It is important to discuss the different types of IUDs and potential side effects with a healthcare provider before choosing an IUD.
Types of IUDs
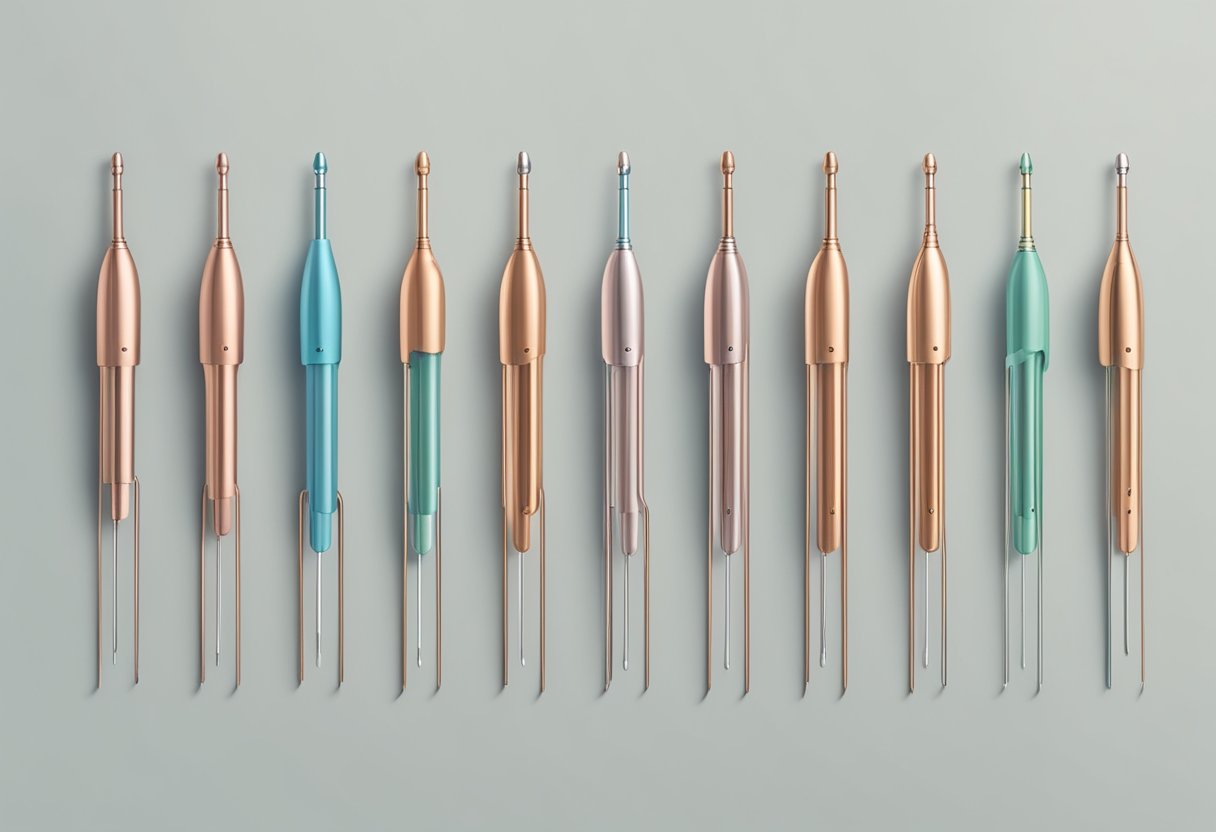
There are two main types of IUDs: Copper IUDs and Hormonal IUDs. Both types of IUDs are highly effective at preventing pregnancy, with a failure rate of less than 1%.
Copper IUDs
Copper IUDs, such as Paragard, are made of copper and plastic. They do not contain any hormones and work by releasing copper ions that prevent fertilization. Copper IUDs can be left in place for up to 10 years and are a good option for women who cannot or do not want to use hormonal birth control.
Hormonal IUDs
Hormonal IUDs, such as Mirena, Kyleena, Liletta, and Skyla, release a small amount of progestin hormone into the uterus. This hormone thickens the cervical mucus, making it difficult for sperm to reach the egg. It also thins the lining of the uterus, making it less likely for a fertilized egg to implant. Hormonal IUDs can be left in place for 3-5 years, depending on the specific type.
Mirena, Kyleena, Liletta, and Skyla are all hormonal IUDs that differ in size, shape, and hormone dosage. Mirena is the largest and contains the highest amount of hormone, while Skyla is the smallest and contains the lowest amount of hormone. Kyleena and Liletta fall in between Mirena and Skyla in terms of size and hormone dosage.
In conclusion, both Copper and Hormonal IUDs are highly effective at preventing pregnancy and can provide long-term, hassle-free contraception. Women should speak with their healthcare provider to determine which type of IUD is best for their individual needs.
Mechanism of Action
IUDs work by preventing sperm from fertilizing an egg, thus preventing pregnancy. There are two main types of IUDs: copper IUDs and hormonal IUDs.
Copper as a Spermicide
Copper IUDs work as a spermicide by releasing copper ions into the uterus. Copper ions are toxic to sperm, preventing them from fertilizing an egg. Additionally, the copper IUD causes an inflammatory response in the uterus, which also prevents fertilization.
Hormonal IUDs and Cervical Mucus
Hormonal IUDs, on the other hand, work by releasing a hormone called progestin. Progestin thickens the cervical mucus, making it difficult for sperm to reach the egg. This hormone also thins the lining of the uterus, making it difficult for a fertilized egg to implant.
Overall, both copper and hormonal IUDs are highly effective at preventing pregnancy. Copper IUDs have a failure rate of 0.8%, while hormonal IUDs have a failure rate of 0.2%. It is important to note that IUDs do not protect against ually transmitted infections, so it is still important to use a barrier method of contraception, such as a condom, to prevent the spread of STIs.
Benefits and Effectiveness
Contraceptive Efficacy
IUDs are one of the most effective forms of birth control available. According to Planned Parenthood, they are more than 99% effective at preventing pregnancy. This makes them as effective as sterilization and the birth control implant. IUDs are a great option for those who want long-term birth control without having to worry about taking a pill every day or using other forms of contraception.
IUDs work by preventing fertilization of the egg by sperm. They do this by releasing either copper or hormones (progestin) into the uterus, which changes the environment and makes it difficult for sperm to survive. Hormonal IUDs also thicken cervical mucus, which makes it difficult for sperm to enter the uterus.
Non-Contraceptive Benefits
In addition to being highly effective at preventing pregnancy, IUDs also offer several non-contraceptive benefits. Copper IUDs can be used as emergency contraception if inserted within five days of unprotected . They can also provide a long-term solution for those who experience heavy periods, as copper is a natural anti-inflammatory. Hormonal IUDs can help regulate periods, making them lighter and more regular. They can also be used to treat conditions such as endometriosis and uterine fibroids.
It is important to note that while IUDs have many benefits, they may not be the right choice for everyone. Those who have a history of pelvic inflammatory disease or certain types of cancer may not be able to use IUDs. It is important to discuss all options with a healthcare provider to determine the best form of birth control for individual needs.
Potential Side Effects and Risks
Common Side Effects
While intrauterine devices (IUDs) are highly effective at preventing pregnancy, they can also cause some side effects. Common side effects include cramping, bleeding, and irregular periods. Hormonal IUDs may also cause headaches, nausea, and breast tenderness.
In most cases, these side effects are mild and go away on their own within a few months. However, if they persist or become severe, it is recommended to consult a healthcare provider.
Serious Complications
While rare, serious complications can occur with IUD use. Pelvic inflammatory disease (PID) is a potential risk associated with IUD use. PID is an infection of the reproductive organs that can cause pain, fever, and other symptoms. If left untreated, PID can lead to infertility.
Ectopic pregnancy is another potential complication of IUD use. This occurs when a fertilized egg implants outside of the uterus, typically in the fallopian tube. Ectopic pregnancy can be life-threatening and requires immediate medical attention.
Expulsion and perforation are also rare but serious complications of IUD use. Expulsion occurs when the IUD falls out of the uterus, while perforation occurs when the IUD punctures the uterine wall. Both of these complications can cause pain and may require surgical intervention.
It is important to note that while these complications are rare, they can be serious. Women considering IUD use should discuss the potential risks and benefits with their healthcare provider before making a decision.
Considerations for Use
Who Should Consider an IUD
IUDs are a good option for people who want long-term, highly effective birth control. They are also a good choice for people who do not want to use hormonal birth control or who have trouble remembering to take a daily pill. However, IUDs are not a good choice for everyone.
People who have a history of pelvic inflammatory disease (PID) or who have an active ually transmitted infection (STI) should not use an IUD. Additionally, people who have a history of uterine cancer or who have an abnormal uterine lining may not be good candidates for an IUD.
Factors Influencing IUD Selection
When choosing an IUD, there are several factors to consider. These include:
-
Lifestyle: People who are very active or who participate in contact sports may be more likely to experience dislodgement or expulsion of the IUD. Additionally, people who have a history of pelvic pain may not be good candidates for an IUD.
-
Risks: All IUDs carry some risks, including the risk of infection, perforation of the uterus, and ectopic pregnancy. People who have a history of liver disease or who are allergic to the materials used in the IUD should not use this form of birth control.
-
Uterine lining: The type of IUD chosen may depend on the thickness of the uterine lining. Hormonal IUDs may be more effective for people with a thin uterine lining, while copper IUDs may be more effective for people with a thick uterine lining.
Overall, IUDs are a highly effective form of birth control that can provide long-term protection against pregnancy. However, it is important to consider all of the factors listed above when choosing an IUD to ensure that it is the right choice for you.






